Unit 1. Introduction to Health Equity Data Science#
The intended audience for this resource is researcher operating within the public health space. However, it also seeks to benefit those with a particular knowledge gap, such as more traditional statisticians new to Artificial Intelligence (AI) methods or more experienced data science practitioners who may be newer to considerations within public health research.
This resource is intended to educate its readers about health equity issues that may be a result of existing bias within data sets and that may be perpetuated due to technical methods such as AI and statistics. For instance, a 2019 study found that a commercial AI model used for tracking and managing health risk in the population was racially biased, with sicker Black patients categorized at the same risk level as healthier White patients [Obermeyer et al., 2019].
The ubiquitous nature of AI technologies has led the broader research community to take a hard look at the impacts of AI bias and ways it can be mitigated [Mehrabi et al., 2021]. Moreover, many organizations are seeking ways to manage the risks AI poses. For example, following a direction from Congress in January 2023, the National Institute of Standards and Technology (NIST) released an AI Resource Management Framework (RMF) to act as a source of practical guidance for conducting responsible AI practices stating: “With proper controls, AI systems can mitigate and manage inequitable outcomes.” In a similar spirit, we aim for these materials to have the following impacts:
Provide public health researchers with insights and strategies to reduce bias and, as a result, lower health disparities while working with AI methodologies.
Give project managers, or those new to AI methodologies, the confidence that these goals are being met.
This introduction will first provide background for what health equity is, information about existing frameworks and CDC initiatives to understand and control for health equitable outcomes, as well as the overall structure of the educational materials herein.
What is health equity?#
Health equity is the state in which everyone has a fair and just opportunity to attain their highest level of health. Achieving this requires ongoing societal efforts to:
Address historical and contemporary injustices.
Overcome economic, social, and other obstacles to health and health care as outlined within the Social Determinants of Health (SDoH), which are the geo-socio-economic conditions that impact our health as we age, live, and work in the world.
Eliminate preventable health disparities. Health disparities are preventable differences in the frequency, intensity, and duration of disease, illness, opportunities, and/or injuries and violence (generally stemming from health inequities) between groups of people.
Levels of the Socio-Ecological Model#
Conventional health approaches tend to examine how to increase healthy behaviors or reduce differences in health between groups of people. Research questions from a health equity perspective ask many of the same questions but add a greater perspective. For example, alongside increasing healthy behaviors, it is important to consider increasing equal access to the social and environmental conditions that can improve health quality and access. The graph below shows components of the Public Health Research Socio-Ecological Model and how an individual’s health equity and behaviors can be influenced by external factors. Note terms shown in the graphic below (e.g. HRSA) can be located in the glossary. A brief explanation of each model component is given below:
Individual: Represents the individual who may be impacted.
Interpersonal: The activities intended to facilitate individual behavior change by affecting social and cultural norms and overcoming individual-level barriers: friends, family, health care providers, community health workers etc.
Organizational: Facilitates individual behavior change by influencing organizational systems and policies such as health care systems, employers or work sites, health care plans, local health departments, tribal urban health clinics, and professional organizations.
Community: Leveraging resources and participation of community-level institutions such as comprehensive cancer control coalitions, tribal health departments, media, and community advocacy groups, which represent potential sources of community communication and support.
Policy: Involves interpreting and implementing existing policy. Federal, state, local, and tribal government agencies may support policies that promote healthy behavior.
CDC and Health Equity#
Disparities in public health have been significantly amplified in recent times. This trend and longstanding health disparities have led the Centers for Disease Control and Prevention (CDC) to prioritize the development of a wide range of health equity interventions. The chart below covers several of the strategies and principles that exist at the CDC today.
Core Strategy |
CDC Health Equity Science Principles (CDC internal use only content) |
Inclusive Communication Principles |
|---|---|---|
Through its CORE strategy, CDC is leading this effort, both in the work done on behalf of the nation’s health and the work performed internally as an organization.
|
|
|
Health Equity Strategies and Public Health#
There is a desire by public health professionals and research communities to develop health equity strategies and integrate them into facilitating health care and research design and development processes. There are two complementary perspectives to consider:
The Avoidance Mindset: Explore and identify biases in analytical workflows that may contribute to health disparities, and then work to mitigate these biases.
The Proactive Mindset: Developing an intentional culture of practice that helps manage risks while enabling analytic workflows to actively address health equity issues.
The Avoidance Mindset:
Many sources of bias can occur within various steps of the research process, from the data curation phase through the dissemination of results. When analyzing a data set, it is important to consider how it was collected, characterize it, and note the potential biases present within. However, once the data set is in hand, the researcher may be unlikely to acquire additional data to correct for missing values or over and under-representation of certain groups. At this juncture it is important for the researcher to understand the limitations of their data source and how this impacts analysis in order to mitigate additional bias. This concerted effort is referred to here as avoidance and means performing research with the intention to avoid reinforcing existing bias and avoid introducing bias that can create health disparities.
The Proactive Mindset:
A proactive mindset requires a holistic approach to addressing health equity concerns within the public health space. The term proactive here means developing a framework that supports the application of best health-equitable practices throughout the research lifecycle and helps to bring awareness to, and enable mitigation (avoidance) strategies, where and when they are needed. A fully realized proactive approach means developing a culture of practicing mindful, health-equitable research by developing health equity strategies that inform every part of the research lifecycle from literature reviews and data source curation, concept and research proposal, and dissemination of results.
These ideas seem to resonate with functions from NIST’s “core” AI RMF, which are denoted as “GOVERN, MAP, MEASURE, and MANAGE”. The proactive approach is outside the scope of this resource. However, these materials provide necessary information and technical tools to support the adoption of a proactive mindset when conducting public health research.
Content Overview#
Why take health equity into consideration?#
The discussion of social determinants of health and the socio-ecological model above illustrates how social, environmental, and economic factors are large contributors to health outcomes for individuals. The environments in which people live affect their health and can introduce health disparities that may be shaped by public policies and health infrastructure, access to education and public transportation, exposure to neighborhood violence, or the existence of social networks. The identification of social determinants of health represents community and even nationwide issues. However, there is evidence that these enormous challenges to public health are not insurmountable and can be mitigated through community efforts and public policy.
Public health research and analyses are often leveraged as the basis for public policy decisions and community interventions in an effort to understand and improve public health. New research efforts reference literature reviews and rely on processing data sources which are all potential carriers of historical bias, demonstrating a precedence problem for health equity. As public health policies are increasingly informed by quantitative approaches and complex technical methods, there is a need for an intentional approach to incorporate health equitable practices into public health research.
Objectives of this Resource#
As a part of its health equity strategy, the CDC aims to utilize AI in data modernization efforts across their data science and surveillance sectors. The incorporation of AI into CDC workflows will require measures to identify, understand, and mitigate potential biases that may arise from the data and the analytic methods in order to reduce negative impacts arising from analysis outcomes.
It is our hope that this resource enables best practices of avoidance, or mitigation of health inequities when developing technical solutions within the public health research space. Incorporating a health equity strategy into data-driven problem-solving means applying a set of best practices that can:
Bring awareness to existing biases (data-centric).
Determine how bias can enter analytic workflows (method-centric).
Recommend best practices to help mitigate health disparities and minimize harm.
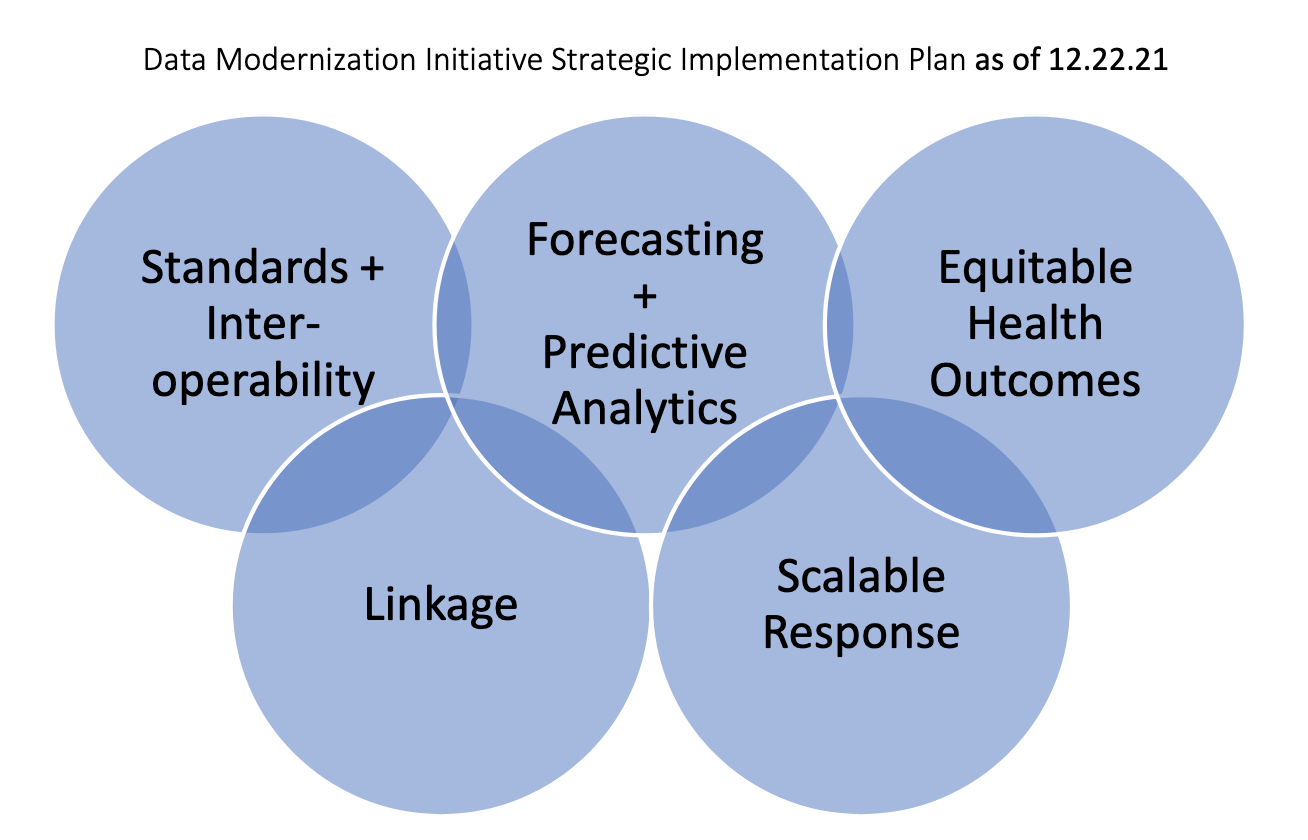
The lessons contained within closely align with stages of the Data Modernization Initiative (DMI), with a focus on strengthening forecasting and predictive analytics by adopting next-generation technologies to produce evidence-based solutions with equitable health outcomes:
Unit Structure#
There are many opportunities for bias to persist throughout the data and research life cycle. This resource defines common types of bias for different phases in the analytic workflow and how each bias may present health equity challenges in public health research. Counter to the social determinants of health and the socio-ecological model, the types of biases discussed in this resource are artifacts from the technical processes of gathering data and performing analyses and require their own mitigation measures. The diagram below gives a high-level idea of the identification of potential bias in different stages of the analytic workflow:

See each unit to access more detailed lessons: